Presented at The Pregnancy Meeting, San Franscisco, CA
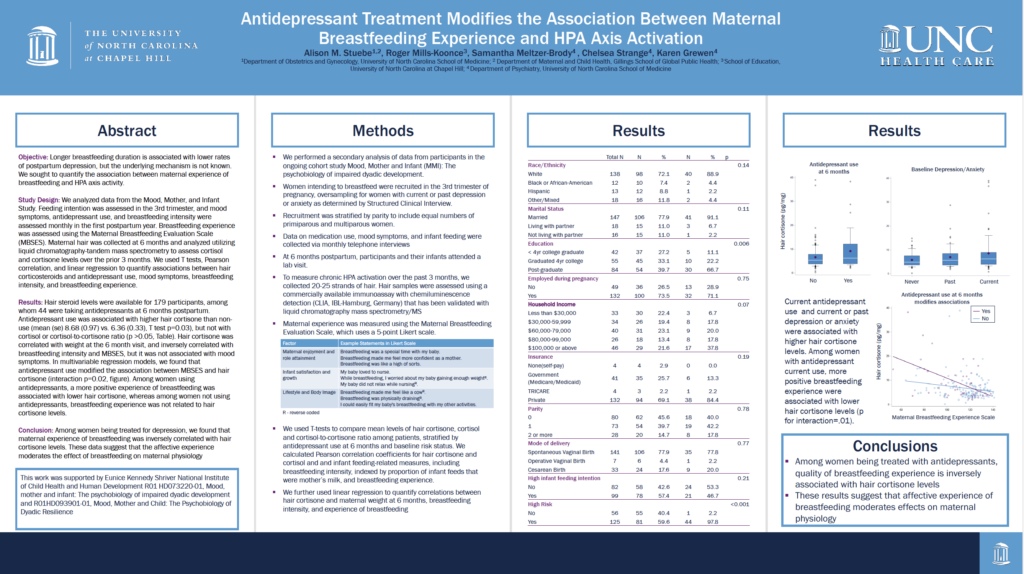
Alison M. Stuebe, Roger Mills-Koonce, Samantha Meltzer-Brody, Chelsea Strange, Karen Grewen
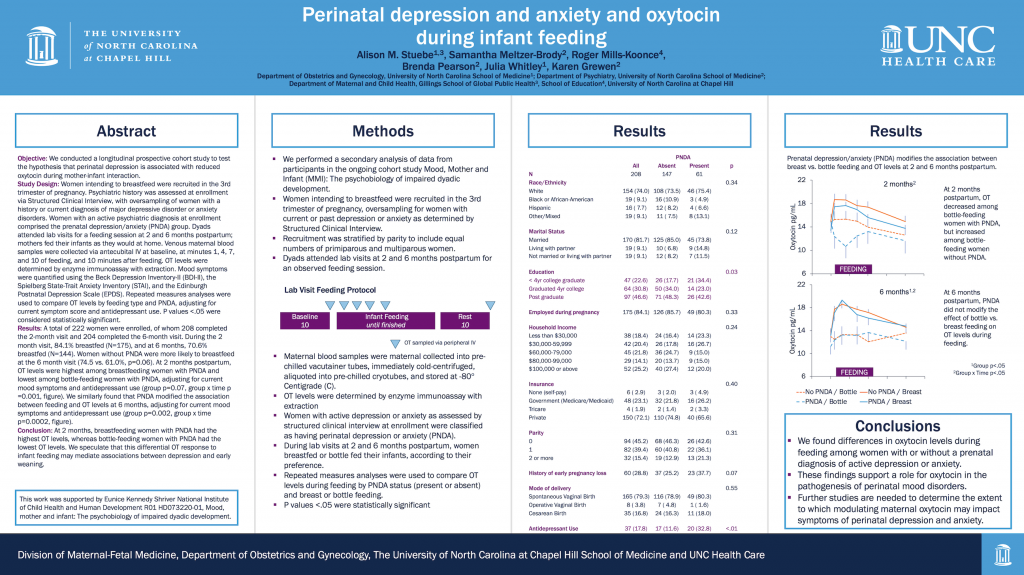
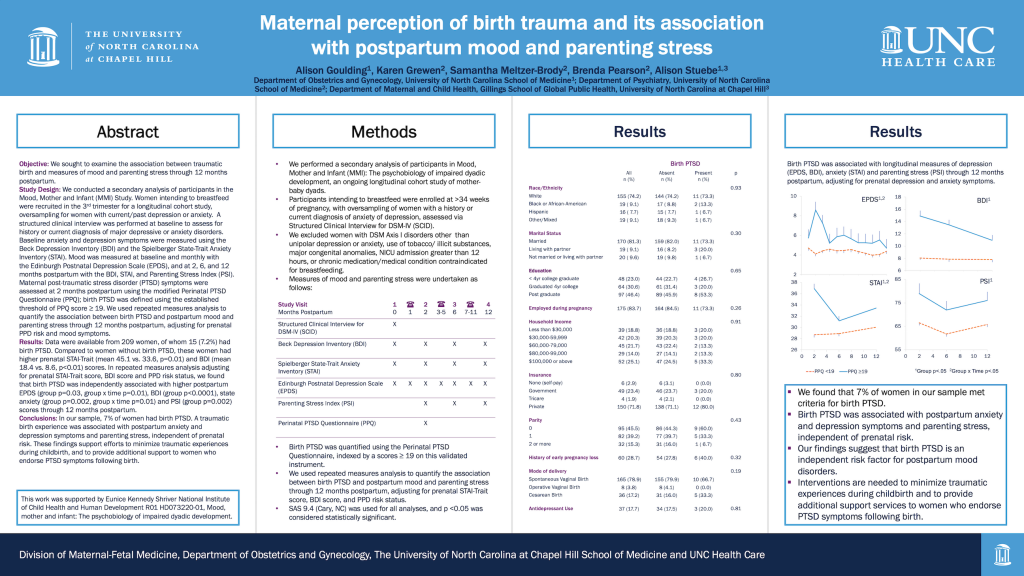
Objective: Longer breastfeeding duration is associated with lower rates of postpartum depression, but the underlying mechanism is not known. We sought to quantify the association between maternal experience of breastfeeding and HPA axis activity.
Study Design: We analyzed data from the Mood, Mother, and Infant Study. Feeding intention was assessed in the 3rd trimester, and mood symptoms, antidepressant use, and breastfeeding intensity were assessed monthly in the first postpartum year. Breastfeeding experience was assessed using the Maternal Breastfeeding Evaluation Scale (MBSES). Maternal hair was collected at 6 months and analyzed utilizing liquid chromatography-tandem mass spectrometry to assess cortisol and cortisone levels over the prior 3 months. We used T tests, Pearson correlation, and linear regression to quantify associations between hair corticosteroids and antidepressant use, mood symptoms, breastfeeding intensity, and breastfeeding experience.
Results: Hair steroid levels were available for 179 participants, among whom 44 were taking antidepressants at 6 months postpartum. Antidepressant use was associated with higher hair cortisone than non-use (mean (se) 8.68 (0.97) vs. 6.36 (0.33), T test p=0.03), but not with cortisol or cortisol-to-cortisone ratio (p >0.05, Table). Hair cortisone was correlated with weight at the 6 month visit, and inversely correlated with breastfeeding intensity and MBSES, but it was not associated with mood symptoms. In multivariable regression models, we found that antidepressant use modified the association between MBSES and hair cortisone (interaction p=0.02, figure). Among women using antidepressants, a more positive experience of breastfeeding was associated with lower hair cortisone, whereas among women not using antidepressants, breastfeeding experience was not related to hair cortisone levels.
Conclusion: Among women being treated for depression, we found that maternal experience of breastfeeding was inversely correlated with hair cortisone levels. These data suggest that the affective experience moderates the effect of breastfeeding on maternal physiology.