Presented at the Society for Maternal Fetal Medicine, Las Vegas, NV, February 2019.
Alison M. Stuebe, Samantha Meltzer-Brody, Roger Mills-Koonce, Brenda Pearson, Julia Whitley, Karen Grewen
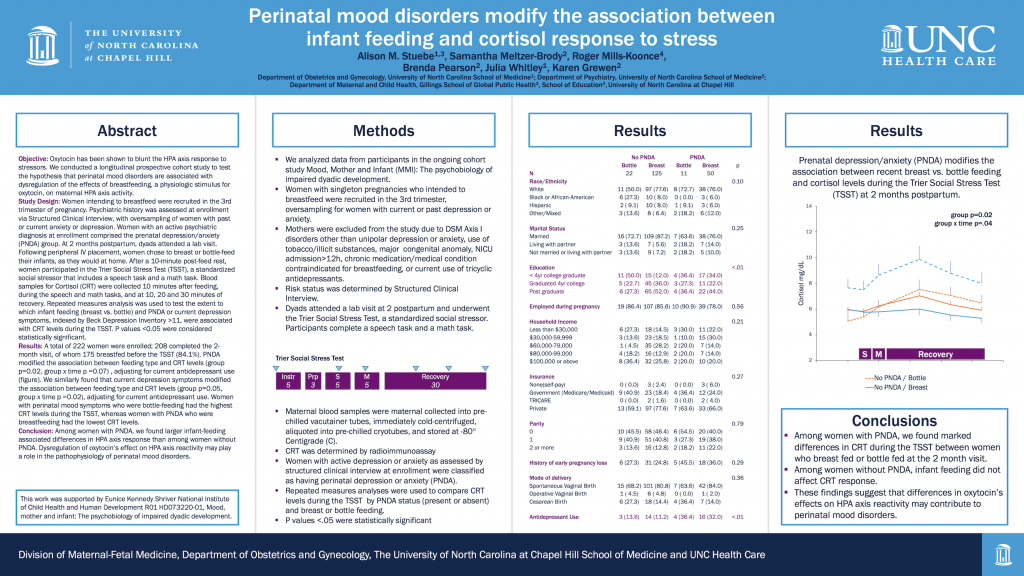
Objective: Oxytocin has been shown to blunt the HPA axis response to stressors. We conducted a longitudinal prospective cohort study to test the hypothesis that perinatal mood disorders are associated with dysregulation of the effects of breastfeeding, a physiologic stimulus for oxytocin, on maternal HPA axis activity.
Study Design: Women intending to breastfeed were recruited in the 3rd trimester of pregnancy. Psychiatric history was assessed at enrollment via Structured Clinical Interview, with oversampling of women with past or current anxiety or depression. Women with an active psychiatric diagnosis at enrollment comprised the prenatal depression/anxiety (PNDA) group. At 2 months postpartum, dyads attended a lab visit. Following peripheral IV placement, women chose to breast or bottle-feed their infants, as they would at home. After a 10-minute post-feed rest, women participated in the Trier Social Stress Test (TSST), a standardized social stressor that includes a speech task and a math task. Blood samples for Cortisol (CRT) were collected 10 minutes after feeding, during the speech and math tasks, and at 10, 20 and 30 minutes of recovery. Repeated measures analysis was used to test the extent to which infant feeding (breast vs. bottle) and PNDA or current depression symptoms, indexed by Beck Depression Inventory >11, were associated with CRT levels during the TSST. P values <0.05 were considered statistically significant.
Results: A total of 222 women were enrolled; 208 completed the 2-month visit, of whom 175 breastfed before the TSST (84.1%). PNDA modified the association between feeding type and CRT levels (group p=0.02, group x time p =0.07) , adjusting for current antidepressant use (figure). We similarly found that current depression symptoms modified the association between feeding type and CRT levels (group p=0.05, group x time p =0.02), adjusting for current antidepressant use. Women with perinatal mood symptoms who were bottle-feeding had the highest CRT levels during the TSST, whereas women with PNDA who were breastfeeding had the lowest CRT levels.
Conclusion: Among women with PNDA, we found larger infant-feeding associated differences in HPA axis response than among women without PNDA. Dysregulation of oxytocin’s effect on HPA axis reactivity may play a role in the pathophysiology of perinatal mood disorders.