Presented at the Breastfeeding and Feminism International Meeting, Chapel Hill, NC March 2019
Alison M. Stuebe, Samantha Meltzer-Brody, Brenda Pearson, Kathryn Wouk, Karen Grewen
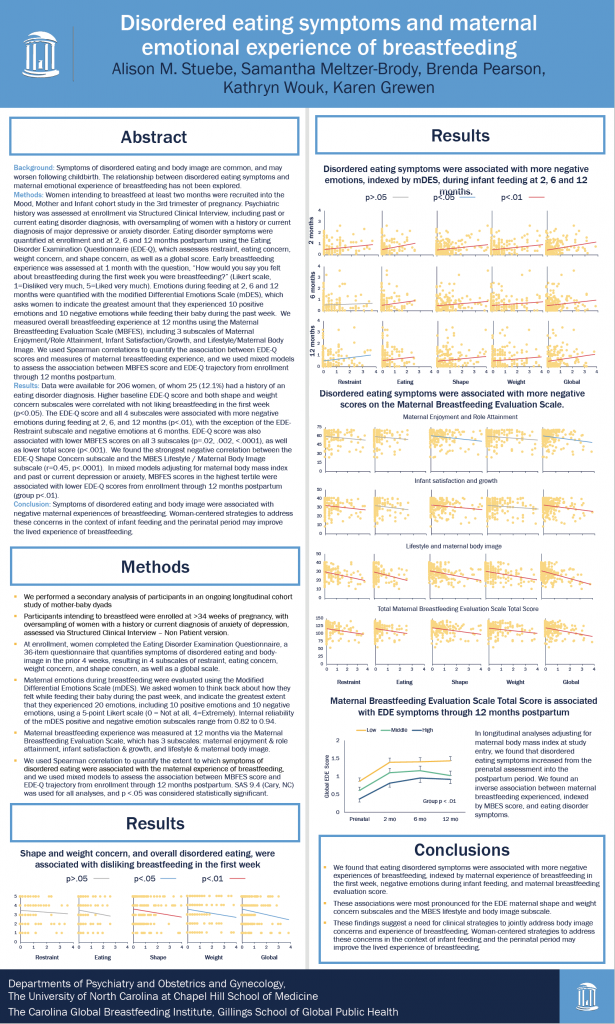
Background: Symptoms of disordered eating and body image are common, and may worsen following childbirth. The relationship between disordered eating symptoms and maternal emotional experience of breastfeeding has not been explored.
Methods: Women intending to breastfeed at least two months were recruited into the Mood, Mother and Infant cohort study in the 3rd trimester of pregnancy. Psychiatric history was assessed at enrollment via Structured Clinical Interview, including past or current eating disorder diagnosis, with oversampling of women with a history or current diagnosis of major depressive or anxiety disorder. Eating disorder symptoms were quantified at enrollment and at 2, 6 and 12 months postpartum using the Eating Disorder Examination Questionnaire (EDE-Q), which assesses restraint, eating concern, weight concern, and shape concern, as well as a global score. Early breastfeeding experience was assessed at 1 month with the question, “How would you say you felt about breastfeeding during the first week you were breastfeeding?” (Likert scale, 1=Disliked very much, 5=Liked very much). Emotions during feeding at 2, 6 and 12 months were quantified with the modified Differential Emotions Scale (mDES), which asks women to indicate the greatest amount that they experienced 10 positive emotions and 10 negative emotions while feeding their baby during the past week. We measured overall breastfeeding experience at 12 months using the Maternal Breastfeeding Evaluation Scale (MBFES), including 3 subscales of Maternal Enjoyment/Role Attainment, Infant Satisfaction/Growth, and Lifestyle/Maternal Body Image. We used Spearman correlations to quantify the association between EDE-Q scores and measures of maternal breastfeeding experience, and we used mixed models to assess the association between MBFES score and EDE-Q trajectory from enrollment through 12 months postpartum.
Results: Data were available for 206 women, of whom 25 (12.1%) had a history of an eating disorder diagnosis. Higher baseline EDE-Q score and both shape and weight concern subscales were correlated with not liking breastfeeding in the first week (p<0.05). The EDE-Q score and all 4 subscales were associated with more negative emotions during feeding at 2, 6, and 12 months (p<.01), with the exception of the EDE-Restraint subscale and negative emotions at 6 months. EDE-Q score was also associated with lower MBFES scores on all 3 subscales (p=.02, .002, <.0001), as well as lower total score (p<.001). We found the strongest negative correlation between the EDE-Q Shape Concern subscale and the MBES Lifestyle / Maternal Body Image subscale (r=0.45, p<.0001). In mixed models adjusting for maternal body mass index and past or current depression or anxiety, MBFES scores in the highest tertile were associated with lower EDE-Q scores from enrollment through 12 months postpartum (group p<.01).
Conclusion: Symptoms of disordered eating and body image were associated with negative maternal experiences of breastfeeding. Woman-centered strategies to address these concerns in the context of infant feeding and the perinatal period may improve the lived experience of breastfeeding.