Presented at the Society for Maternal Fetal Medicine, Las Vegas, NV, February 2019.
 Alison Goulding, Karen Grewen, Samantha Meltzer-Brody, Brenda Pearson, Alison Stuebe
Alison Goulding, Karen Grewen, Samantha Meltzer-Brody, Brenda Pearson, Alison Stuebe
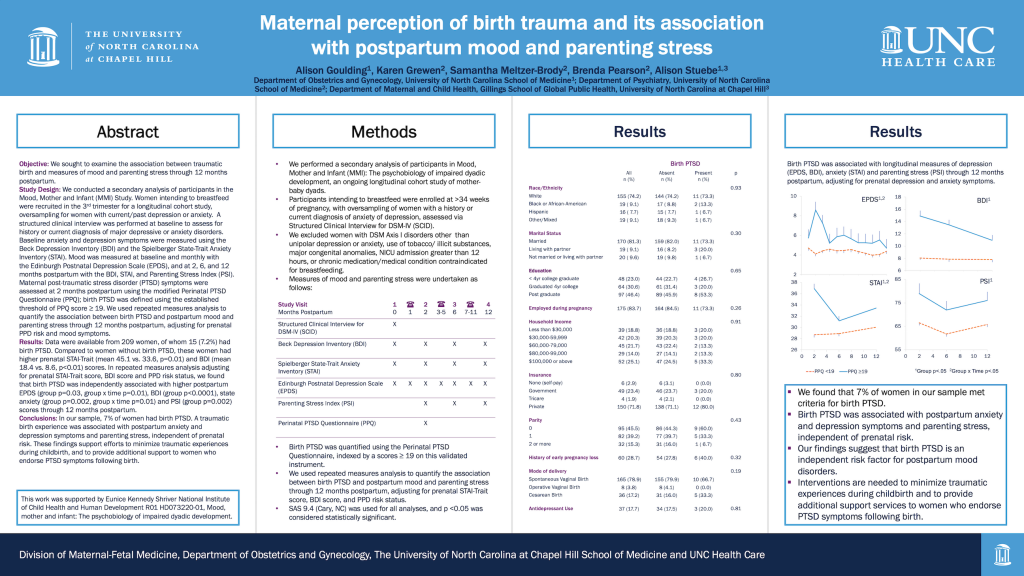
Objective: We sought to examine the association between traumatic birth and measures of mood and parenting stress through 12 months postpartum.
Study Design: We conducted a secondary analysis of participants in the Mood, Mother and Infant (MMI) Study. Women intending to breastfeed were recruited in the 3rdtrimester for a longitudinal cohort study, oversampling for women with current/past depression or anxiety. A structured clinical interview was performed at baseline to assess for history or current diagnosis of major depressive or anxiety disorders. Baseline anxiety and depression symptoms were measured using the Beck Depression Inventory (BDI) and the Spielberger State-Trait Anxiety Inventory (STAI). Mood was measured at baseline and monthly with the Edinburgh Postnatal Depression Scale (EPDS), and at 2, 6, and 12 months postpartum with the BDI, STAI, and Parenting Stress Index (PSI). Maternal post-traumatic stress disorder (PTSD) symptoms were assessed at 2 months postpartum using the modified Perinatal PTSD Questionnaire (PPQ); birth PTSD was defined using the established threshold of PPQ score ≥ 19. We used repeated measures analysis to quantify the association between birth PTSD and postpartum mood and parenting stress through 12 months postpartum, adjusting for prenatal PPD risk and mood symptoms.
Results: Data were available from 209 women, of whom 15 (7.2%) had birth PTSD. Compared to women without birth PTSD, these women had higher prenatal STAI-Trait (mean 45.1 vs. 33.6, p=0.01) and BDI (mean 18.4 vs. 8.6, p<0.01) scores. In repeated measures analysis adjusting for prenatal STAI-Trait score, BDI score and PPD risk status, we found that birth PTSD was independently associated with higher postpartum EPDS (group p=0.03, group x time p=0.01), BDI (group p<0.0001), state anxiety (group p=0.002, group x time p=0.01) and PSI (group p=0.002) scores through 12 months postpartum.
Conclusions: In our sample, 7% of women had birth PTSD. A traumatic birth experience was associated with postpartum anxiety and depression symptoms and parenting stress, independent of prenatal risk. These findings support efforts to minimize traumatic experiences during childbirth, and to provide additional support to women who endorse PTSD symptoms following birth.







